Exit
Article
1/21
Previous
Next
Rally Magazine acknowledges the Wurundjeri people of the Kulin Nation as the Traditional Owners of the land and waterways on which we work and live. We pay our respects to Elders past and present, and to the traditional custodians of all the lands from which our stories and artworks were created.
We recognise Aboriginal and Torres Strait Islanders as the land’s first storytellers and the custodians of the world’s oldest continuous living culture.
Rally Magazine uses the Social Model of Disability when referring to the term ‘disability’.
As defined by People with Disability Australia, "The social model seeks to change society in order to accommodate people with impairment. It does not seek to change persons with impairment to accommodate society."
You can learn more about this model here.
Editorial letter
Welcome to the inaugural issue of Rally Magazine: a multimedia mag on a mission.
Rally was born out of a desire to take action against political apathy. Our team – filled with washed-up student mag editors and designers – knew we wanted to use our storytelling skills to fight back. But the question became: how can we compete in an already oversaturated media landscape? ...
Rally was born out of a desire to take action against political apathy. Our team – filled with washed-up student mag editors and designers – knew we wanted to use our storytelling skills to fight back. But the question became: how can we compete in an already oversaturated media landscape? ...
Read
More
Enter
Article
Read
More
Meet the team

Baya Ou Yang
Co-founder and Editor

Ange Iaria
Co-founder and Creative Director

Sejal Bhikha
Design and Editorial Team

Steph Riordan
Editorial Team

Lynley Eavis
Editorial Team

Baya Ou Yang
Co-founder and Editor

Ange Iaria
Co-founder and
Creative Director

Sejal Bhikha
Design and Editorial Team

Steph Riordan
Editorial Team

Lynley Eavis
Editorial Team

Baya Ou Yang
Co-founder & Editor

Ange Iaria
Co-founder & Creative Director

Sejal Bhikha
Design & Editorial Team

Lynley Eavis
Editorial Team

Steph Riordan
Editorial Team
Meet the Advisory Board

Amity Mara
Advisory Board

Renay Barker-Mulholland
Advisory Board

Josie Young
Advisory Board

Kylie Maslen
Advisory Board

Amity Mara
Advisory Board

Josie Young
Advisory Board

Kylie Maslen
Advisory Board

Renay Barker-Mulholland
Advisory Board

Amity Mara

Josie Young

Kylie Maslen

Renay Barker-Mulholland
Part 1.
Communication
How do we communicate something others can't see?
With Dominique Acciarito, Kaitlyn Blythe, Khadija Gbla, Helene Hill and Iman Rahman
Tap

Illustrations by Katie Zhou
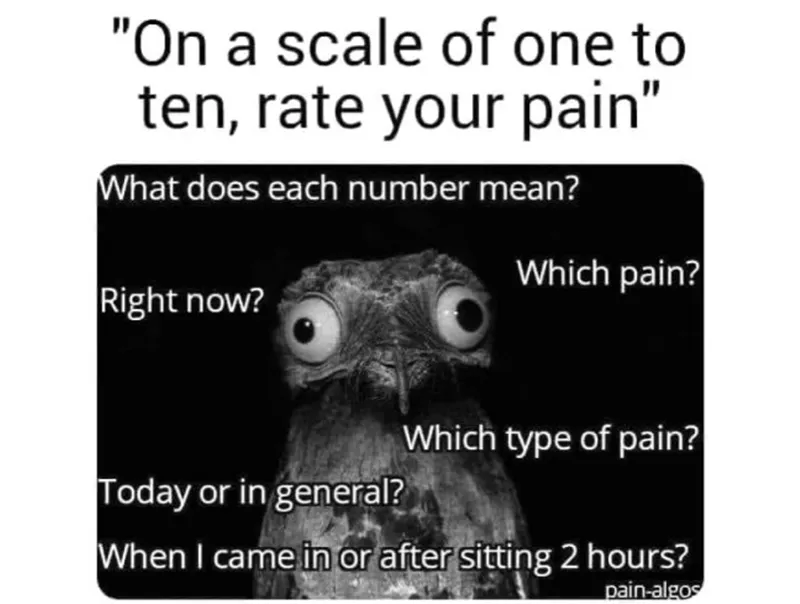
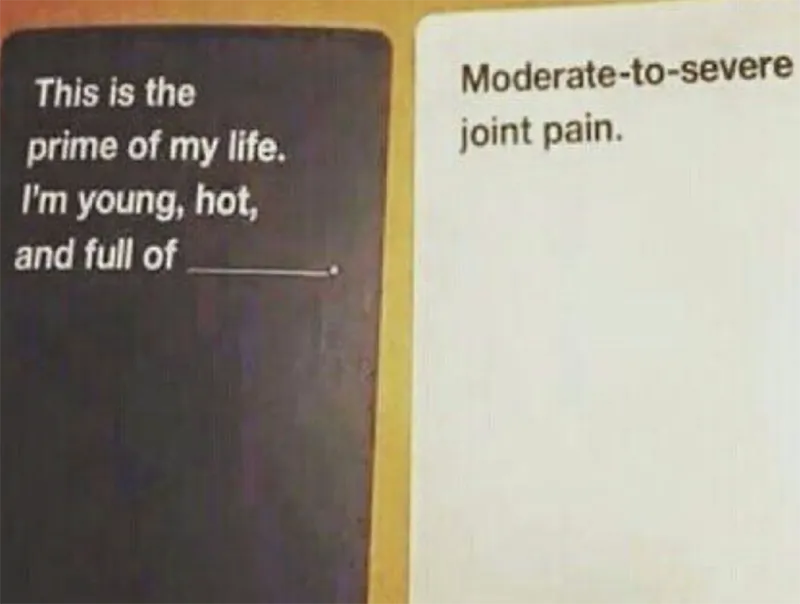
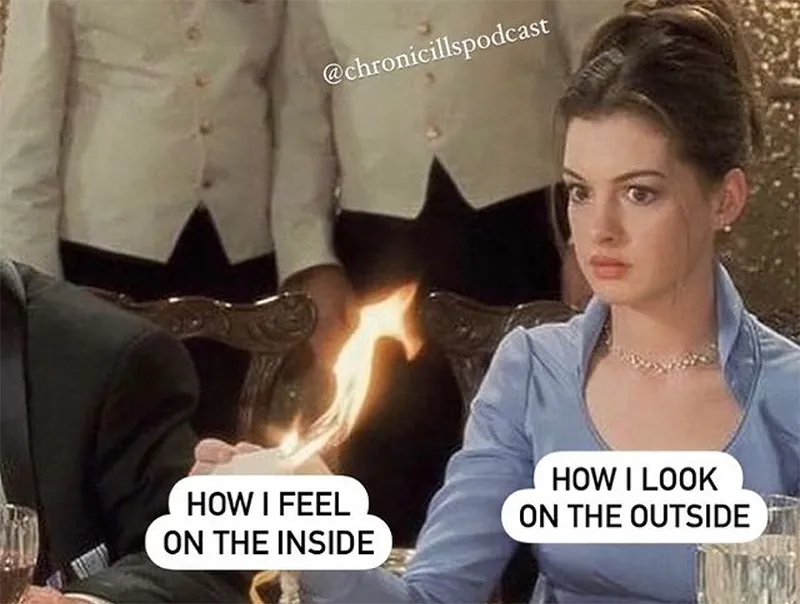
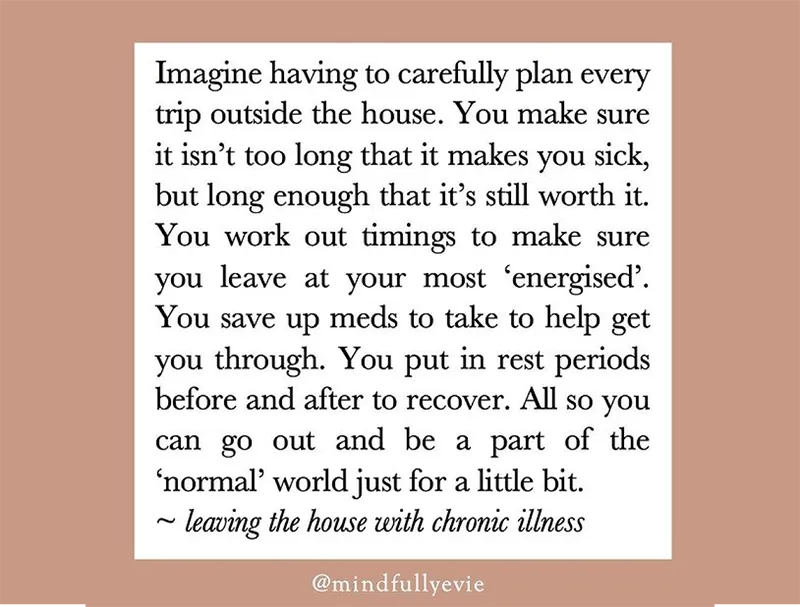
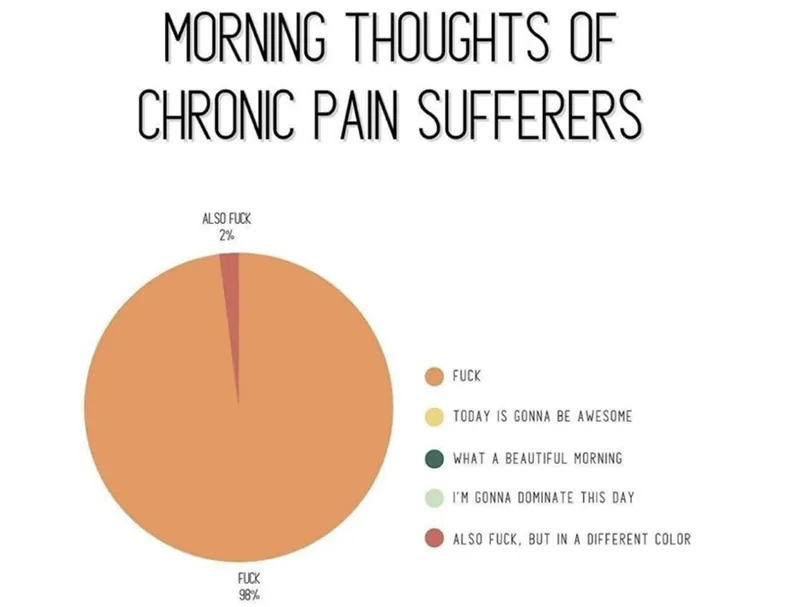
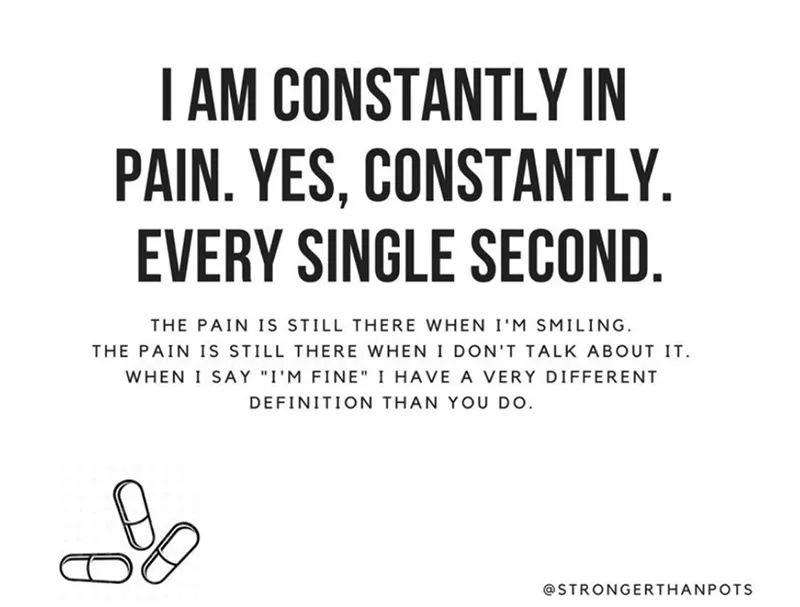
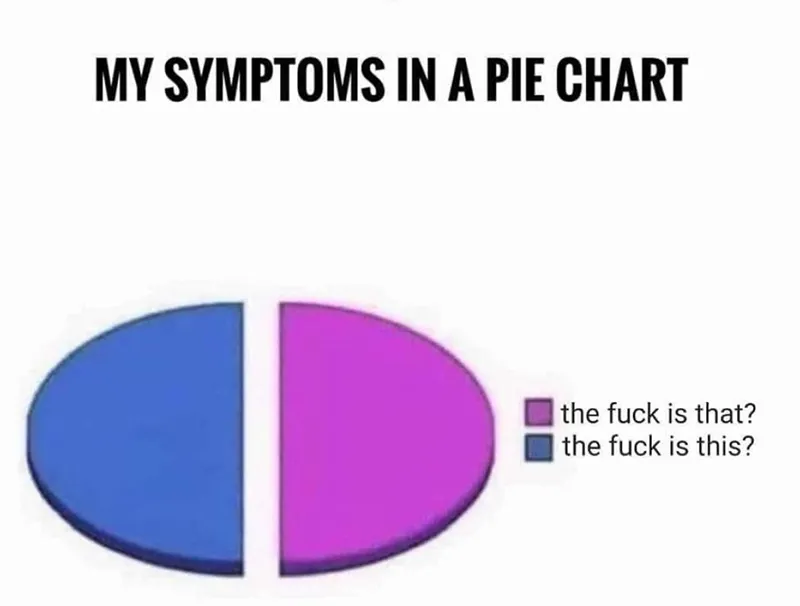
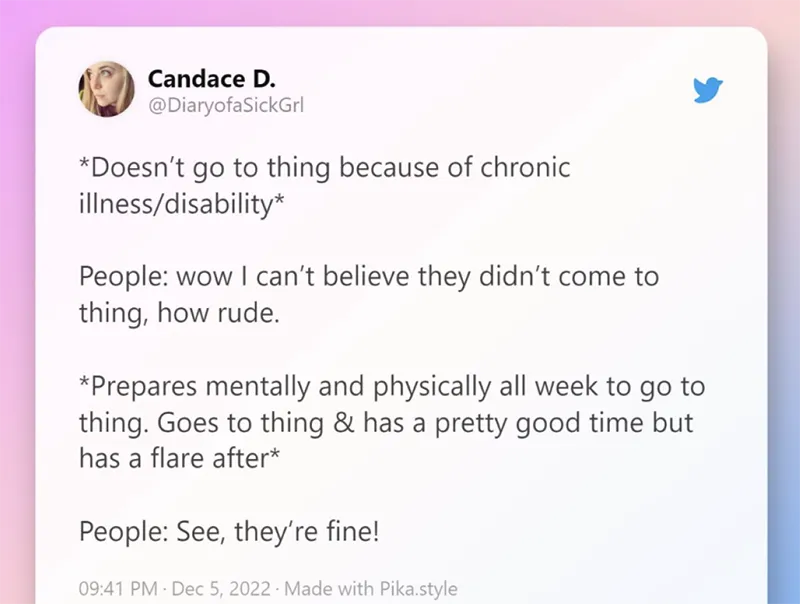
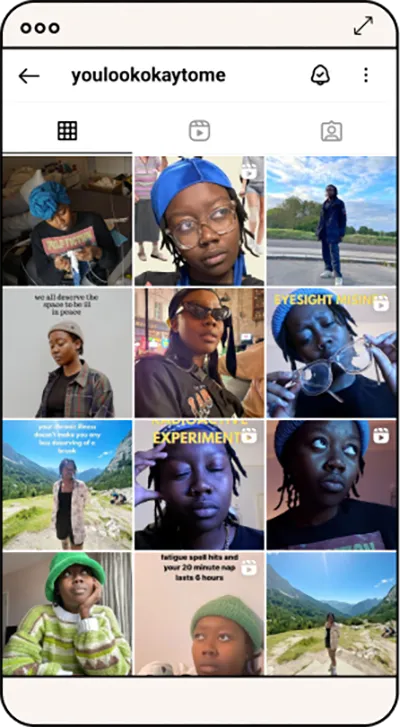
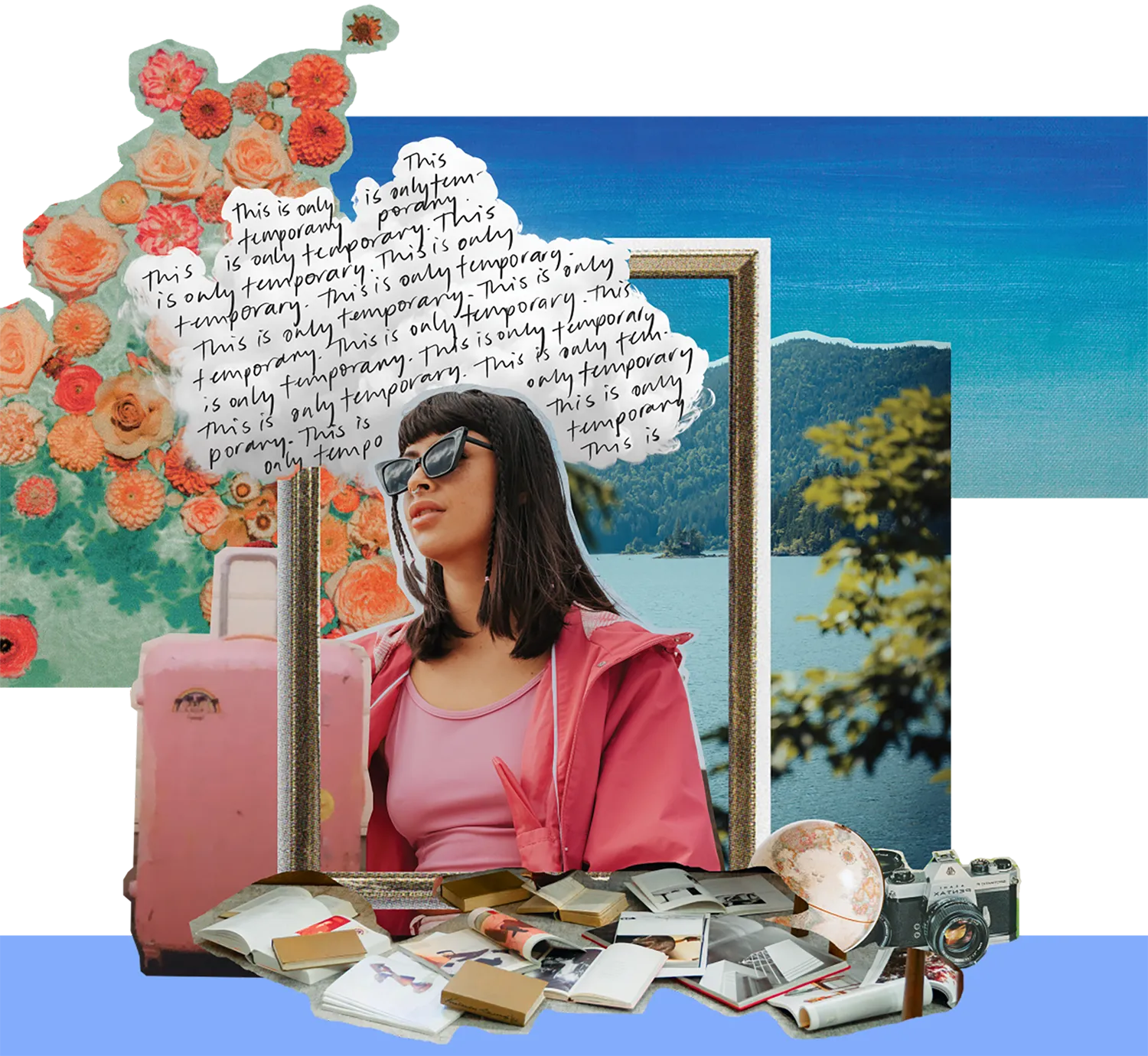
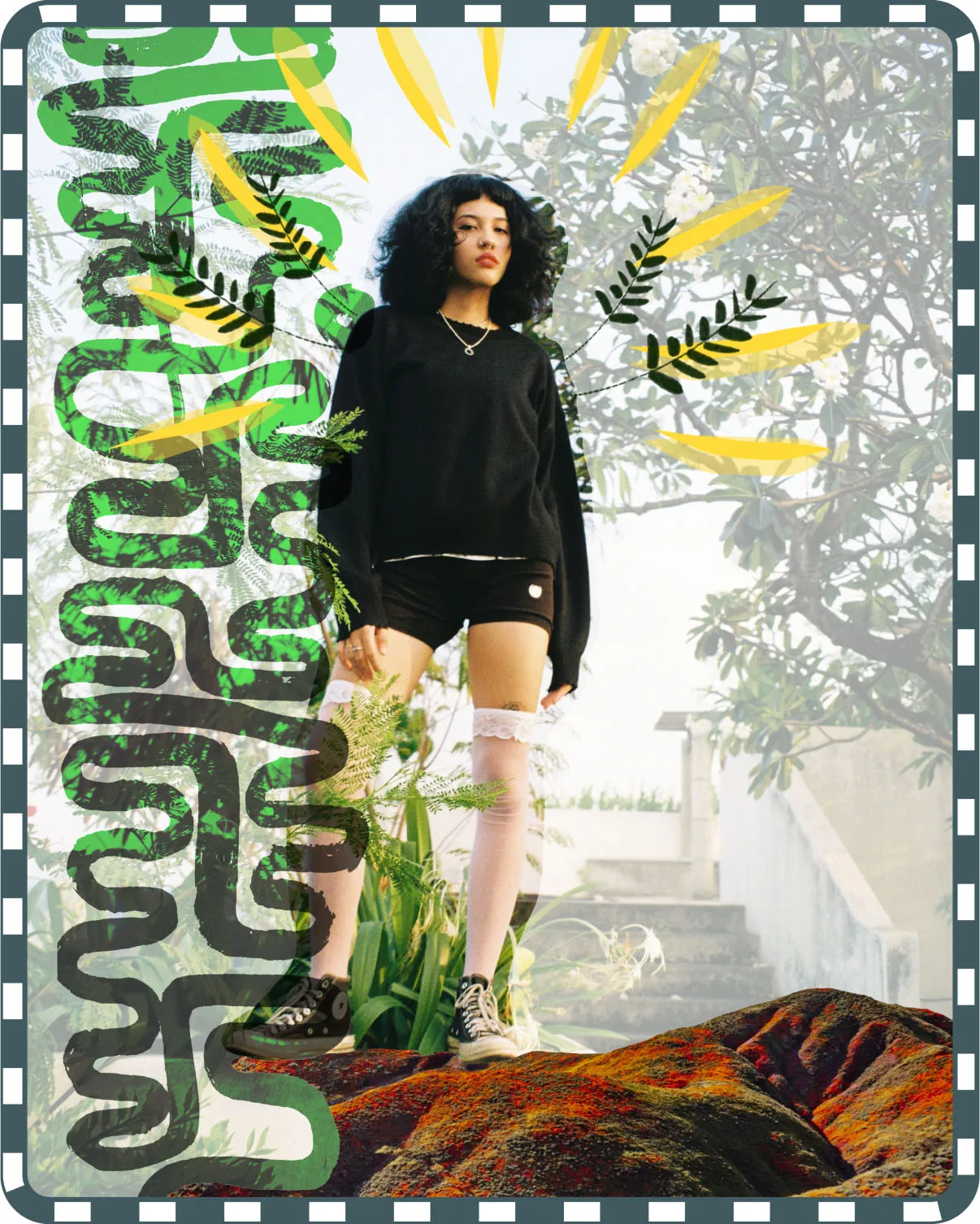
Pain worlds, as coined by Dr Elena Gonzalez-Polledo and described in Kylie Maslen’s book Show Me Where It Hurts, are "corners of social media where those of us suffering from invisible illnesses are able to express ourselves through means more creative than a number."
We take you inside the pain worlds of 4 different content creators.
Tap


Illustrations by Katie Zhou
Pain worlds, as coined by Dr Elena Gonzalez-Polledo and described in Kylie Maslen’s book Show Me Where It Hurts, are "corners of social media where those of us suffering from invisible illnesses are able to express ourselves through means more creative than a number. Selfies, status updates and memes... help to make the pain feel observable, and its chronic nature and symptoms tangible."
We take you inside the pain worlds of 4 different content creators.
We take you inside the pain worlds of 4 different content creators.
There
are
better
ways to
explain
pain
(And the internet is making it possible)
THERE ARE
BETTER WAYS
TO EXPLAIN PAIN
(And the internet is making it possible)
Enter
Article

We can hold two
(competing) truths at once
WORDS BY JULIA BAK
ILLUSTRATIONS BY GRACE TAYLOR
Much of chronic pain is about accepting and honouring contradictory truths. Using words, numbers and labels to explain pain is a crucial part to survival, but they also serve to flatten our experiences. So instead, we learn to straddle these grey areas like a pillow between the thighs.
Much of chronic pain is about accepting and honouring contradictory truths. Using words, numbers and labels to explain pain is a crucial part to survival, but they also serve to flatten our experiences. So instead, we learn to straddle these grey areas like a pillow between the thighs.
Read more
10 minute read

Enter
Article
Enter
Article
Enter
Article
Lou
Wall
The everyday quirks of living with invisible illness as told by our funniest creators.
Lou Wall
The everyday quirks of living with invisible illness as told by our funniest creators.
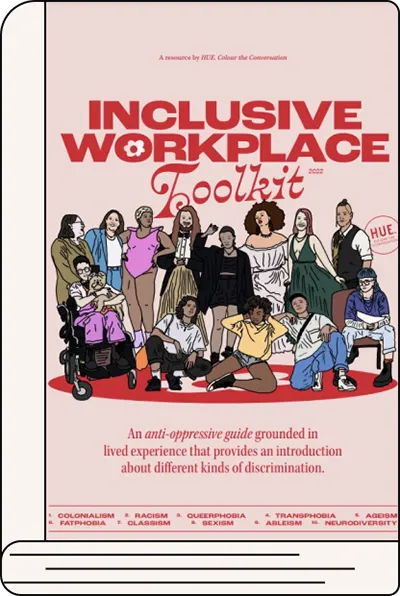
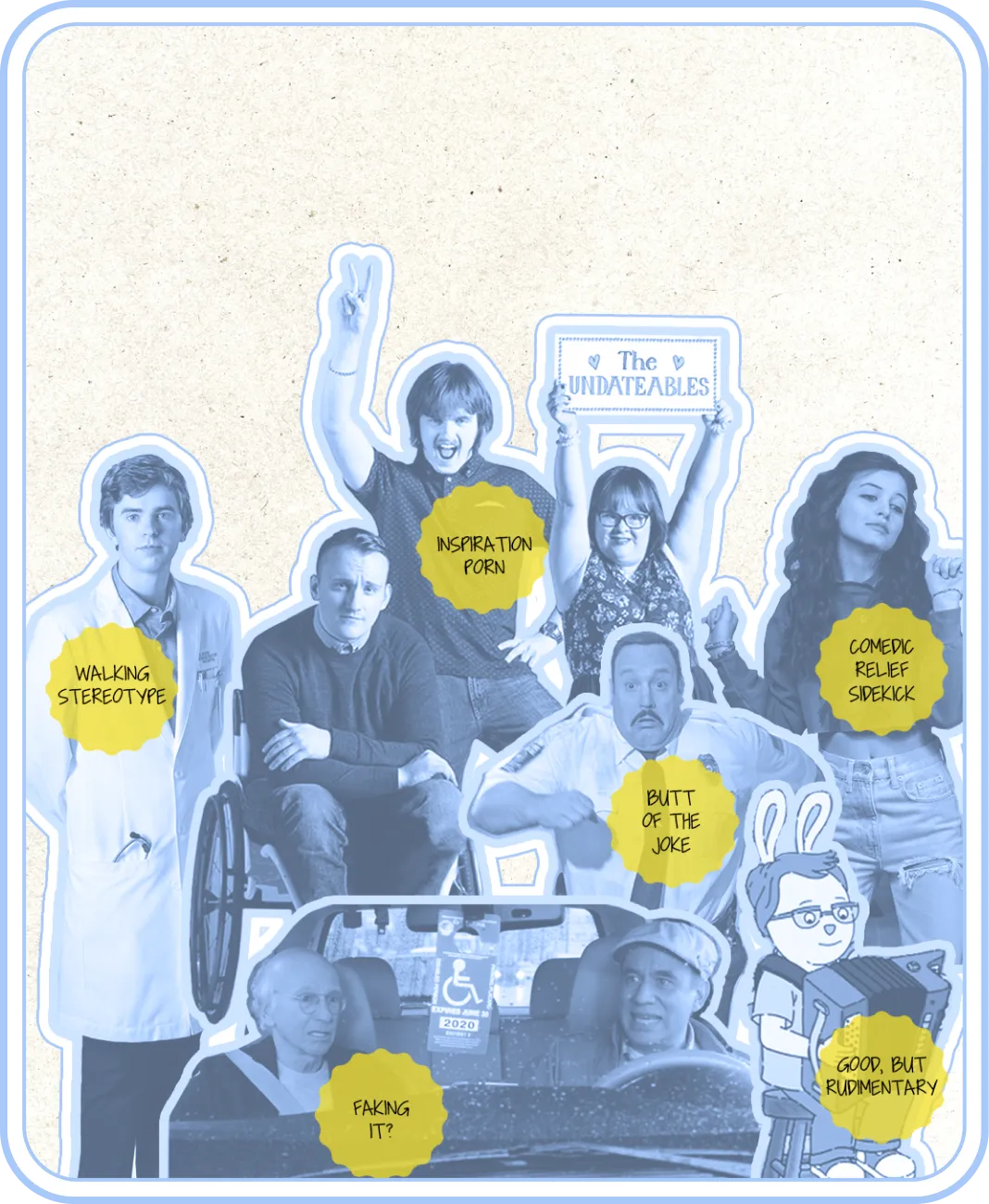
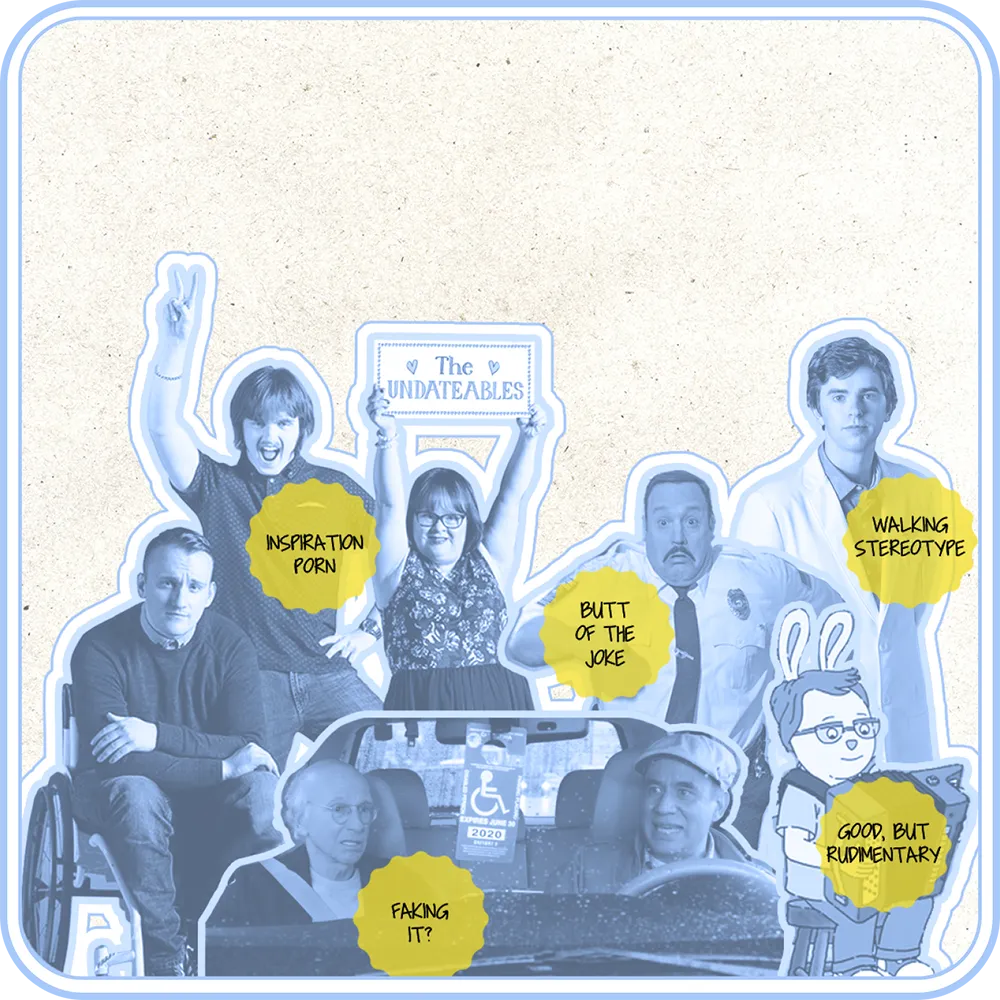
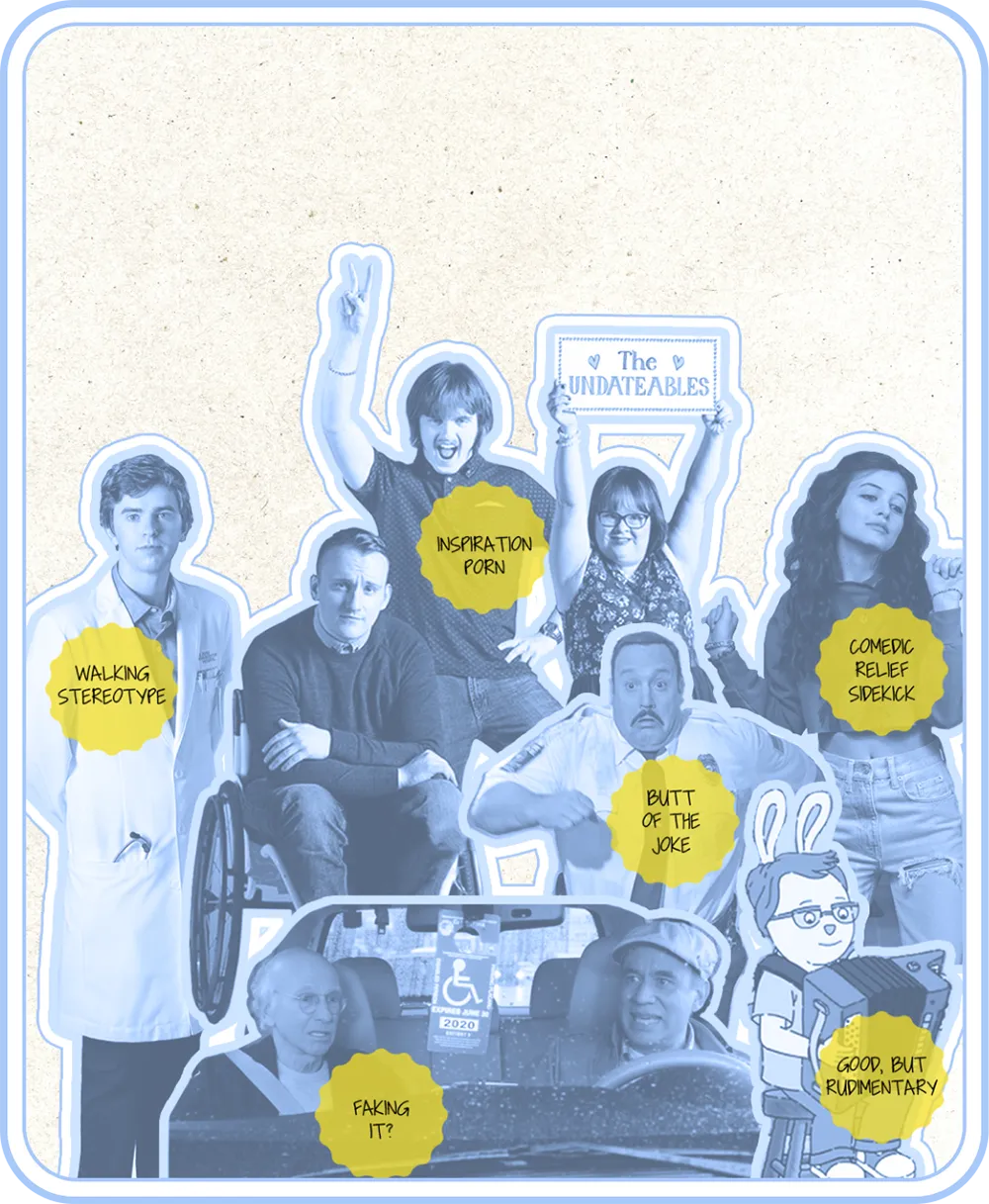
Representation matters:
(unless it sucks)
Words by
Alex Creece
Representation matters! But it counts for crumbs when the portrayals we see are not accurate, sensitive or helpful. What are the harms of misrepresentation in media for people with disability and chronic illness?
Read More
Words by
Alex Creece
Representation matters! But it counts for crumbs when the portrayals we see are not accurate, sensitive or helpful. What are the harms of misrepresentation in media for people with disability and chronic illness?
Read More

Enter
Article
Enter
Article
Enter
Article
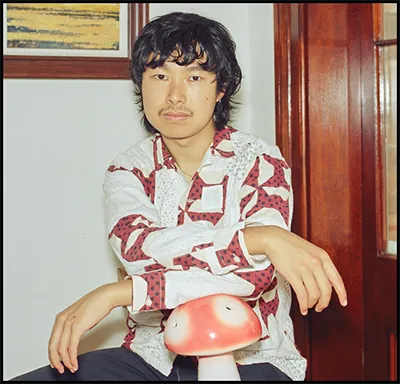
A playlist from
Michael
Sun
Did you know that mediaeval humans used to sleep in two phases? One in the evening, one in the early morning. I know this because I used to Google it all the time when I couldn’t sleep in the middle of the night. I have no idea why I did this; call it delirium. It offered no comfort — I would convince myself the story was merely apocryphal. And, more importantly, we are no longer living in mediaeval times. Disordered sleeping fell out of fashion long ago.
There is no romance to insomnia, despite what Sleepless in Seattle may suggest. Above all, insomnia is not chic; being tired isn’t a personality. Because I am melodramatic, staying up into the dark makes me want to literally die. Nothing to do but push through the roiling hours. 8, 12, then 24 hours awake: a feat of endurance with no medal at the finish line. May this playlist be your reward.
There is no romance to insomnia, despite what Sleepless in Seattle may suggest. Above all, insomnia is not chic; being tired isn’t a personality. Because I am melodramatic, staying up into the dark makes me want to literally die. Nothing to do but push through the roiling hours. 8, 12, then 24 hours awake: a feat of endurance with no medal at the finish line. May this playlist be your reward.
A playlist to listen to when you are going through it, curated by some people who have been through it too.

A playlist to listen to when you are going through it, curated by some people who have been through it too.

A playlist to listen to when you are going through it, curated by some people who have been through it too.

I've got a playlist for that
Something to listen to when you are going through it, curated by people who have been through it too.
Playlist by Michael Sun

read
more
Enter
Article



Part 2.
Systems
How do we communicate something others can't see?
With Sophie Aylmore, Kaitlyn Blythe and Tori Hobbs

Types of medical biases
A guide for understanding how medical biases effect our healthcare
Read more here
Enter
Article
Enter
Article
Enter
Article
Ashley
Apap

The everyday quirks of living with invisible illness as told by our funniest creators.
Ashley Apap
The everyday quirks of living with invisible illness as told by our funniest creators.

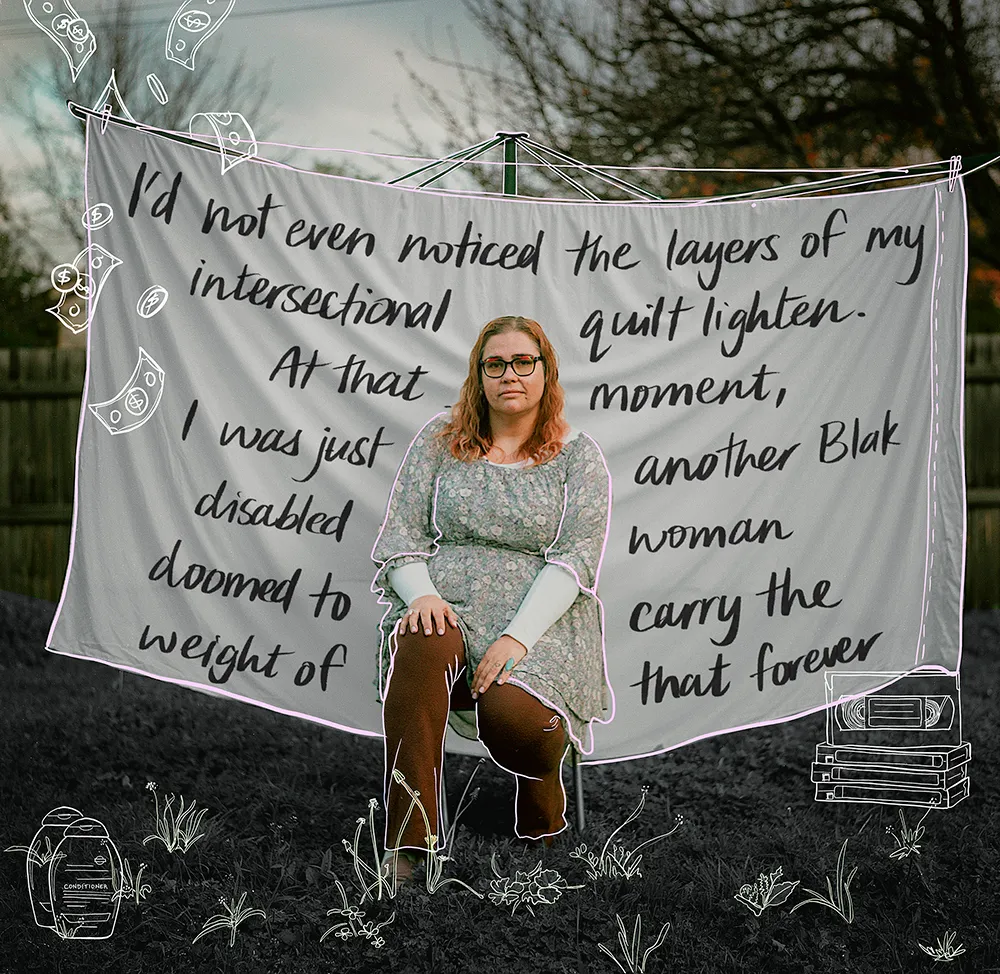
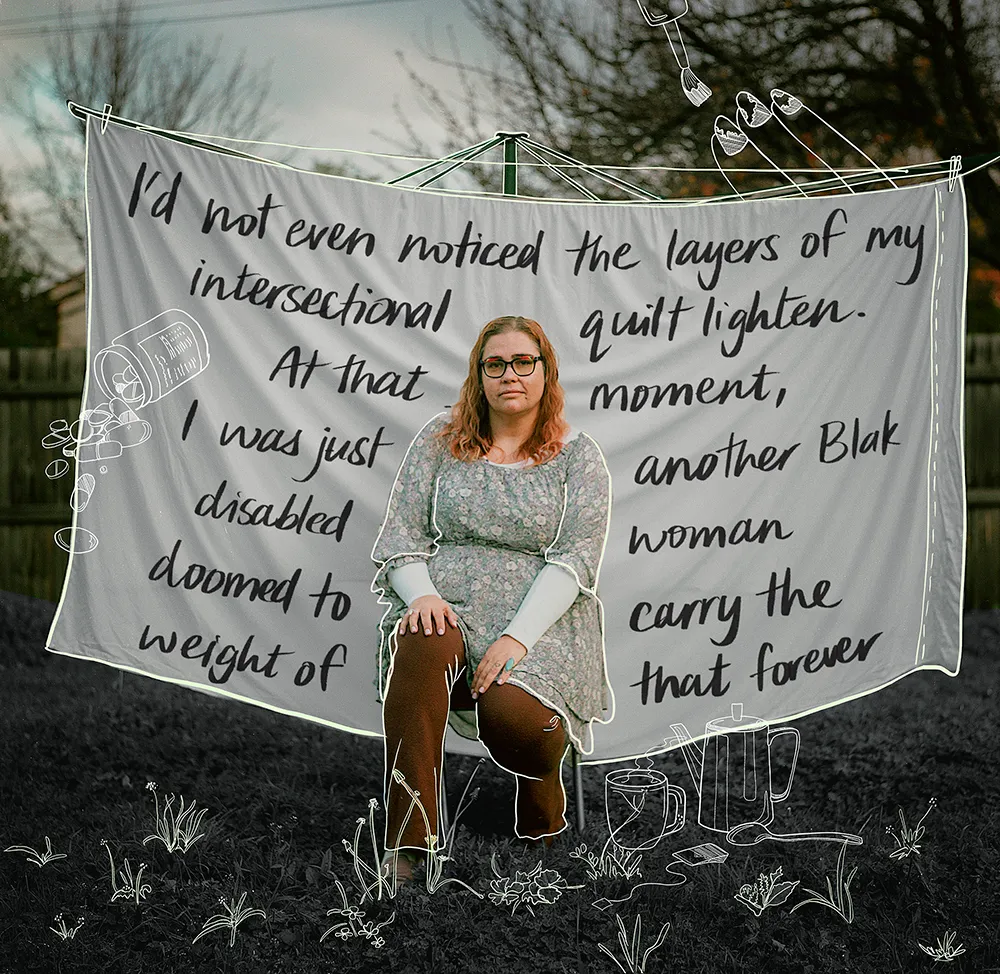
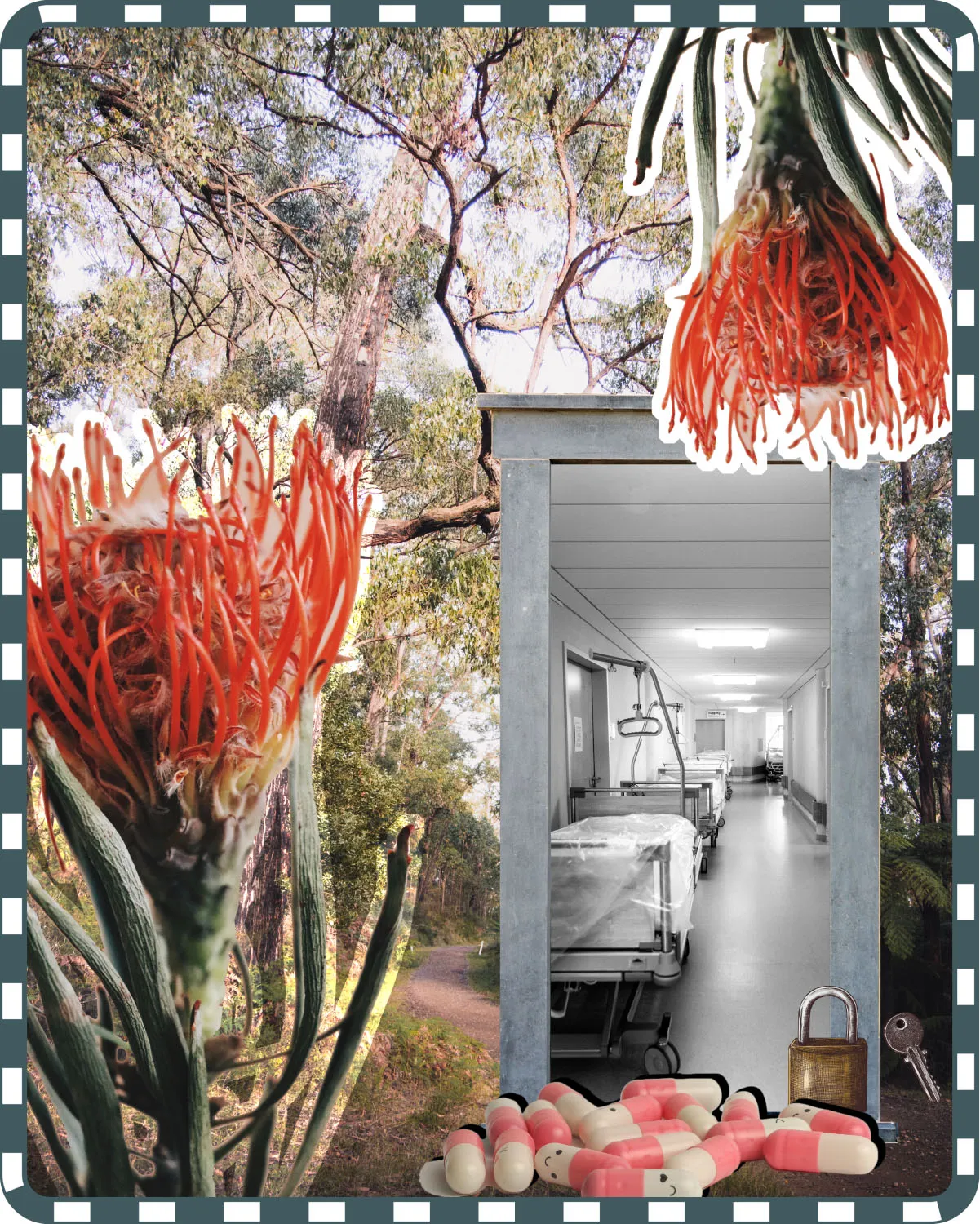
Three people. Three stories. Three generations of trauma trying to survive within the Australian medical system.
The Weight of the Medical System
The Weight of the Medical System
The Weight of the Medical System
Words by Renay Barker-Mulholland
Photos by Em Jensen
The Weight of the Medical System
The Weight of the Medical System
The Weight of the Medical System
Words by Renay Barker-Mulholland
Photos by Em Jensen
read
more
Enter
Article
Enter
Article

A playlist from
Tori Hobbs
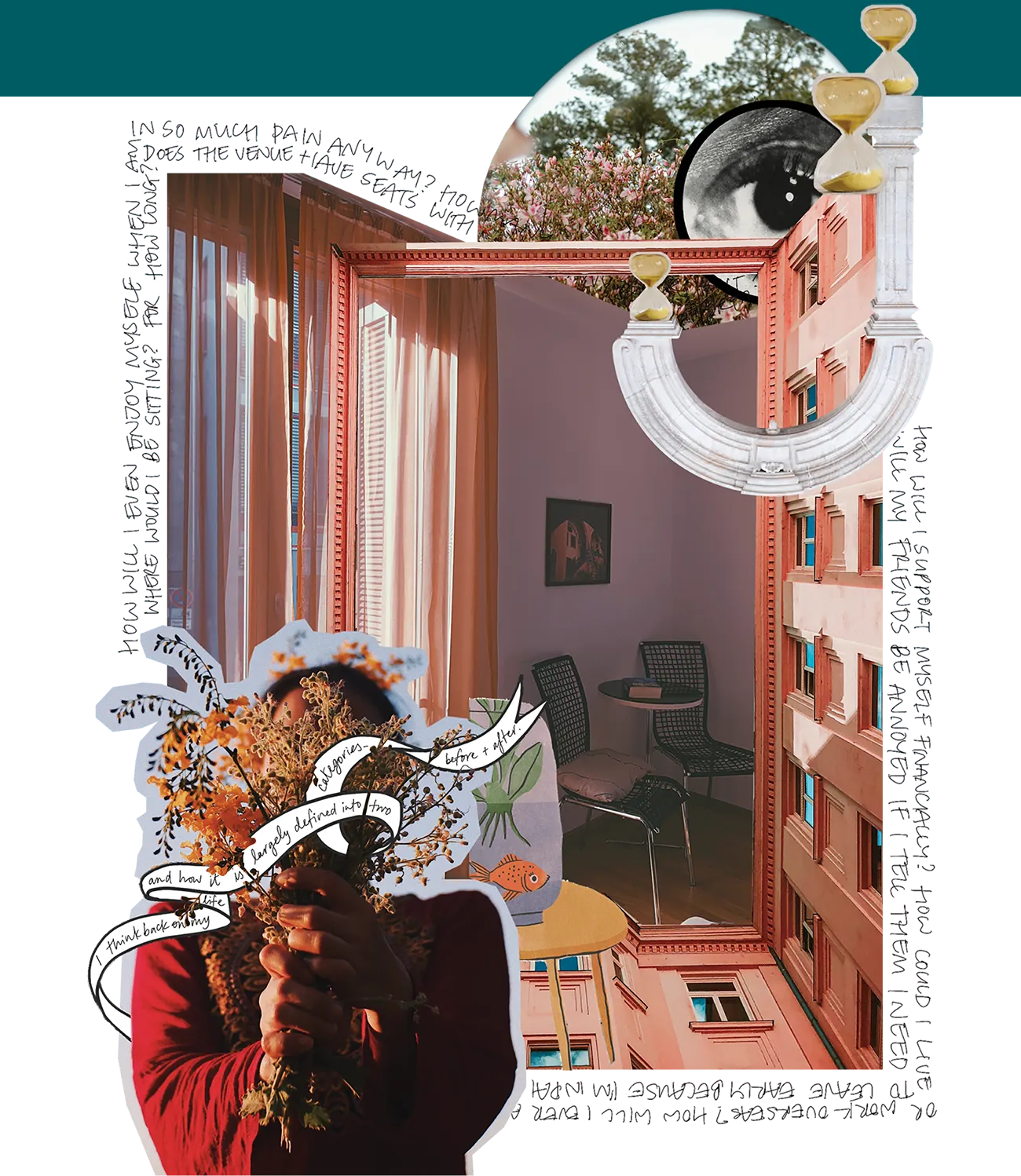
The disabled experience is wide and varied. No two are the same, but we still build worlds and communities around our collective experiences. We recognise our strengths, our unique perspectives, our joy. How we push on despite everything and hold each other, near and far, through it all. When it feels like the rest of the world has left us behind.
This playlist is for all those times you feel isolated, for when you’re invited to your friend's DJ gig but the venue’s inaccessible, for when you shit your pants because all the bathrooms at the train station are closed, for when you’re in the car after a life- changing specialist appointment, for when you’re in line at the chemist transferring money out of your savings account to pay for your medication because it isn’t subsidised by the Pharmaceutical Benefits Scheme (PBS), for when you’ve exhausted all your sick leave at work. For all those moments when you desperately need to dance, or cry it out, or both.
This playlist is for all those times you feel isolated, for when you’re invited to your friend's DJ gig but the venue’s inaccessible, for when you shit your pants because all the bathrooms at the train station are closed, for when you’re in the car after a life- changing specialist appointment, for when you’re in line at the chemist transferring money out of your savings account to pay for your medication because it isn’t subsidised by the Pharmaceutical Benefits Scheme (PBS), for when you’ve exhausted all your sick leave at work. For all those moments when you desperately need to dance, or cry it out, or both.
A playlist to listen to when you are going through it, curated by some people who have been through it too.

A playlist to listen to when you are going through it, curated by some people who have been through it too.

I've got a playlist for that
Something to listen to when you are going through it, curated by people who have been through it too.
Playlist by Tori Hobbs

read
more
Enter
Article
Moments of impact
Words by
Angela Iaria
The journey to understanding, accepting and making space for our own disabilities is long and ongoing. Relief comes from a world that can learn to slow down, listen to and make space for us too.
Content Warning: Car accident, PTSD
LONG READ
The journey to understanding, accepting and making space for our own disabilities is long and ongoing. Relief comes from a world that can learn to slow down, listen to and make space for us too.
Content Warning: Car accident, PTSD
Content Warning: Car accident, PTSD

Enter
Article
Moments of impact
Words by
Angela Iaria
The journey to understanding, accepting and making space for our own disabilities is long and ongoing. Relief comes from a world that can learn to slow down, listen to and make space for us too.
Content Warning: Car accident, PTSD
Content Warning: Car accident, PTSD

Enter
Article
Enter
Article
Enter
Article
Part 3.
Solutions
How do we communicate something others can't see?
With Sophie Aylmore, Kaitlyn Blythe and Tori Hobbs
read
more
Enter
Article

Emilia and Nory have looked to technology, community and creativity in building for themselves alternative ways of living. We were honoured to be invited in their spaces to see and hear it for ourselves.
10 minute read
Alternative ways of living
Interview by Sejal Bhikha
Conversations with Emilia Schnall and Nory Gretz
Photos by Thomas Feng
Emilia and Nory have looked to technology, community and creativity in building for themselves alternative ways of living. We were honoured to be invited in their spaces to see and hear it for ourselves.
10 minute read
Enter
Article

Podcast: Rethinking sick leave
Interviews with Leon Harper, Amity Mara, Kate Marshall and Róisín McGee
Created by Stephanie Riordan
Trying to manage a full-time job while confining the flare-ups of your chronic illness or disability into just ten days of sick leave is a pretty impossible task. In this podcast, we ask the question: Are there better ways to support employees beyond the current model of leave?
Transcript available here.

Podcast: Rethinking sick leave
Created by Stephanie Riordan
Interviews with Leon Harper, Amity Mara, Kate Marshall and Róisín McGee
read
more
Enter
Article
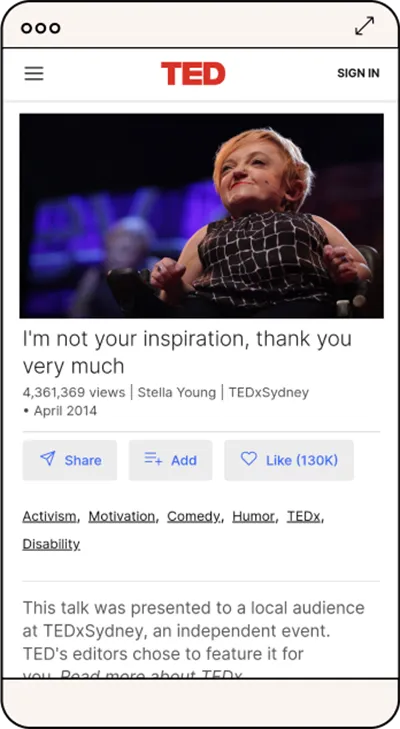
So what comes next?
By reading this issue of Rally Magazine, we hope you have felt a deepening of your understanding for the lives of others and an expanding of your empathy. Please don’t stop here.
There are many resources that helped inform the creation of this issue which we also encourage you to read, watch and listen to. There are many actions you can take into your everyday life to drive positive change for the community we are all a part of.
By reading this issue of Rally Magazine, we hope you have felt a deepening of your understanding for the lives of others and an expanding of your empathy. Please don’t stop here.
There are many resources that helped inform the creation of this issue which we also encourage you to read, watch and listen to. There are many actions you can take into your everyday life to drive positive change for the community we are all a part of.
Enter
Article
read
more
Enter
Article
Take action
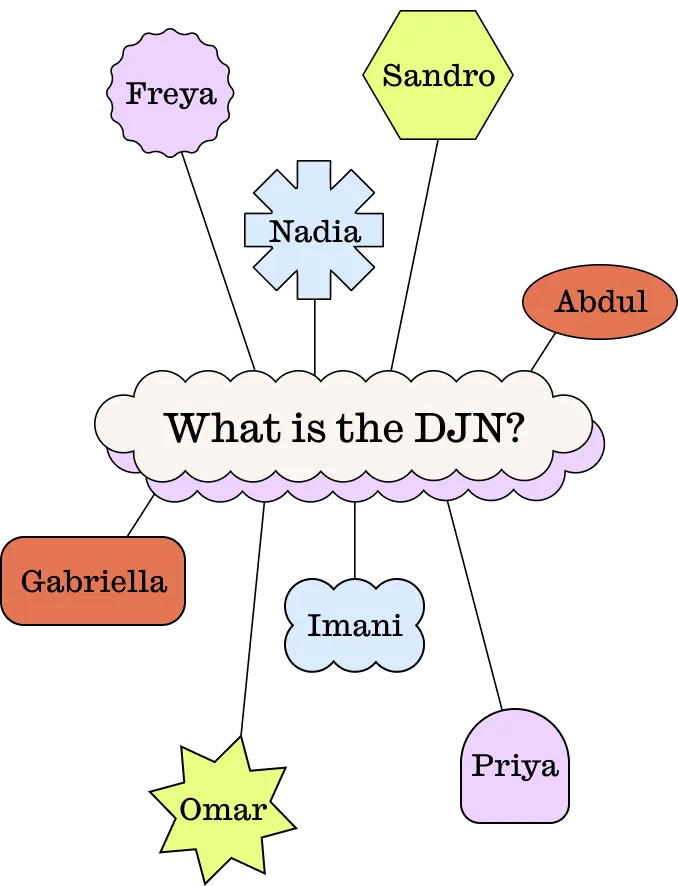
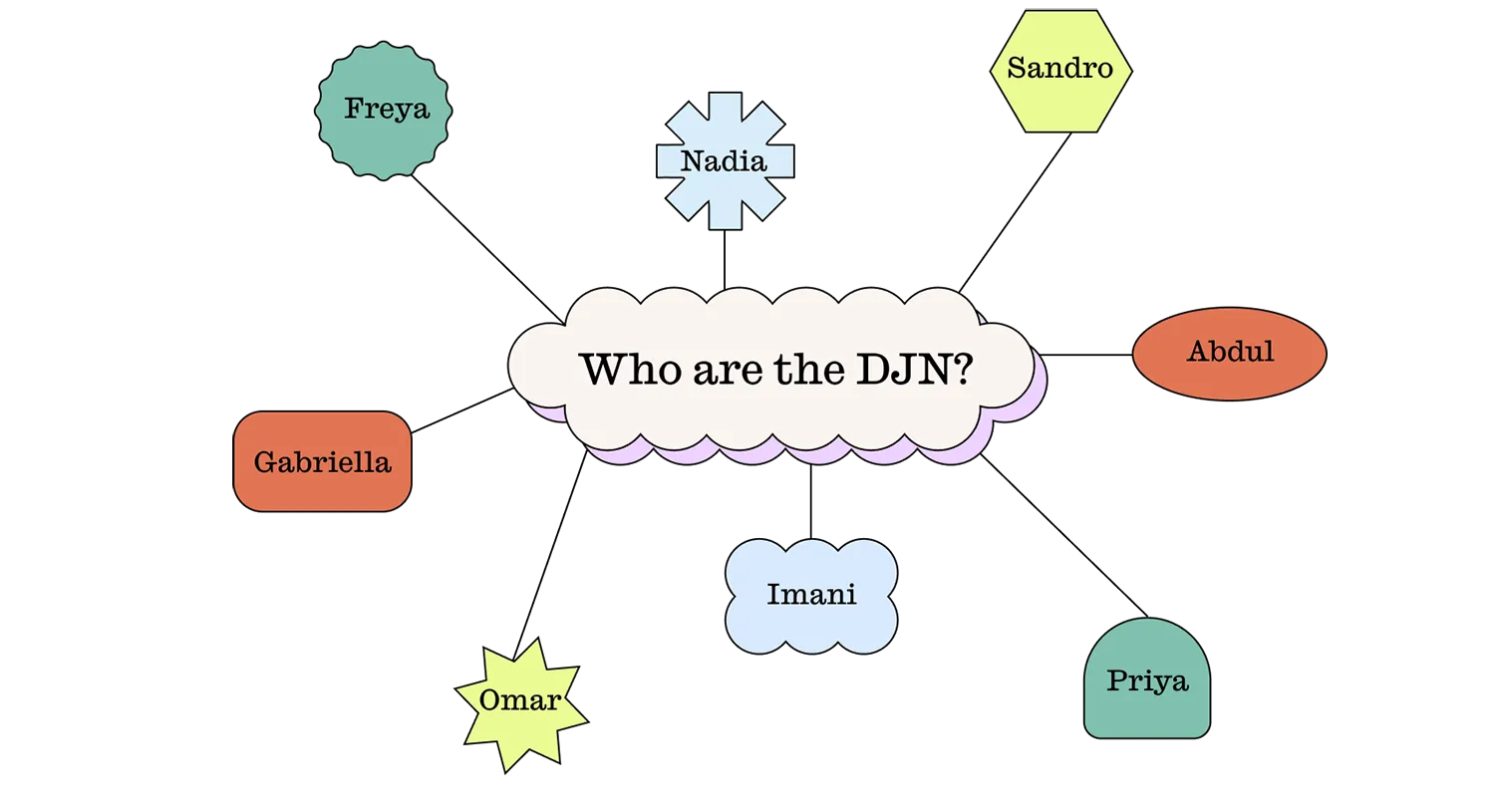
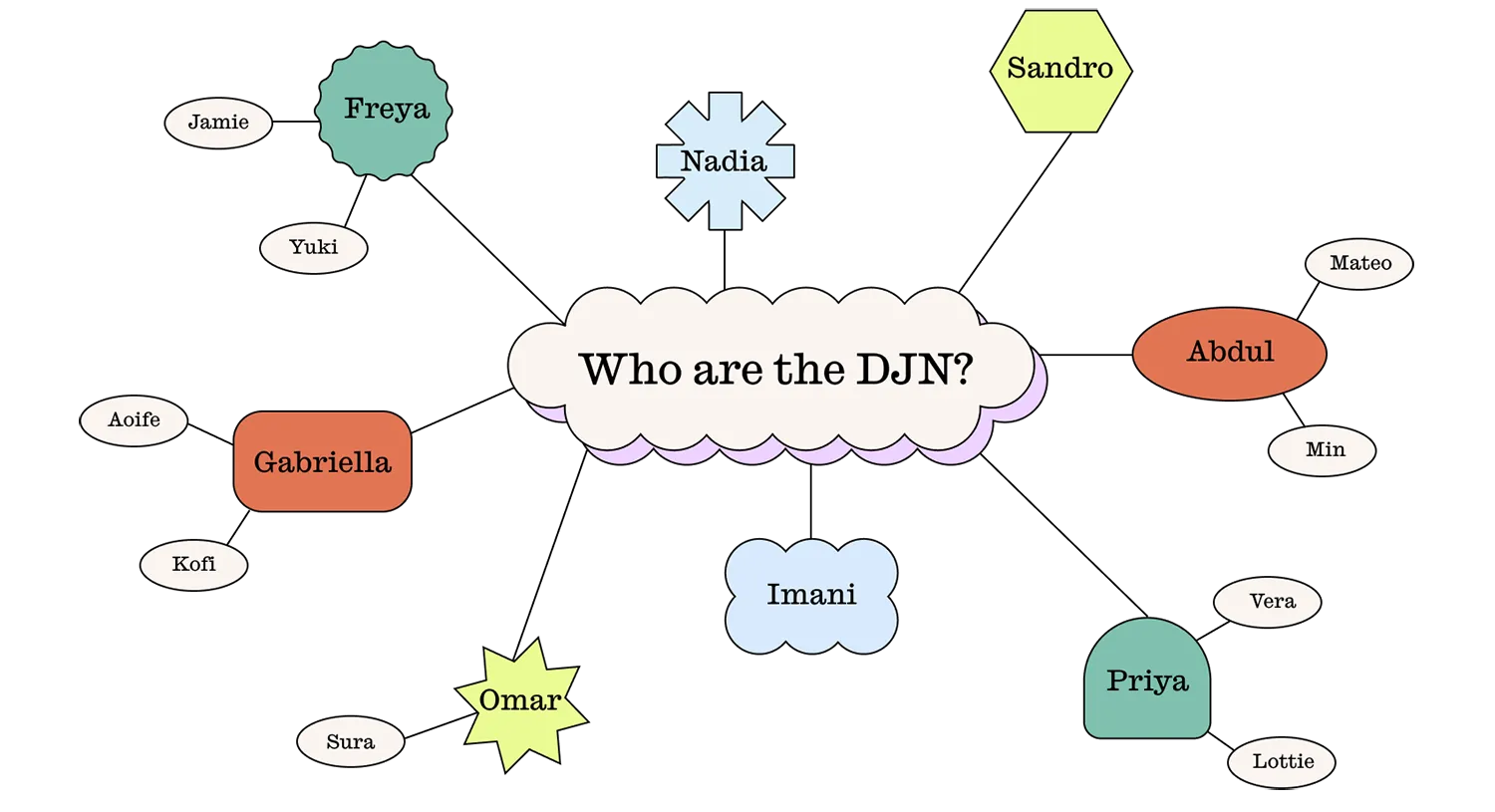
Support the Disability Justice Network
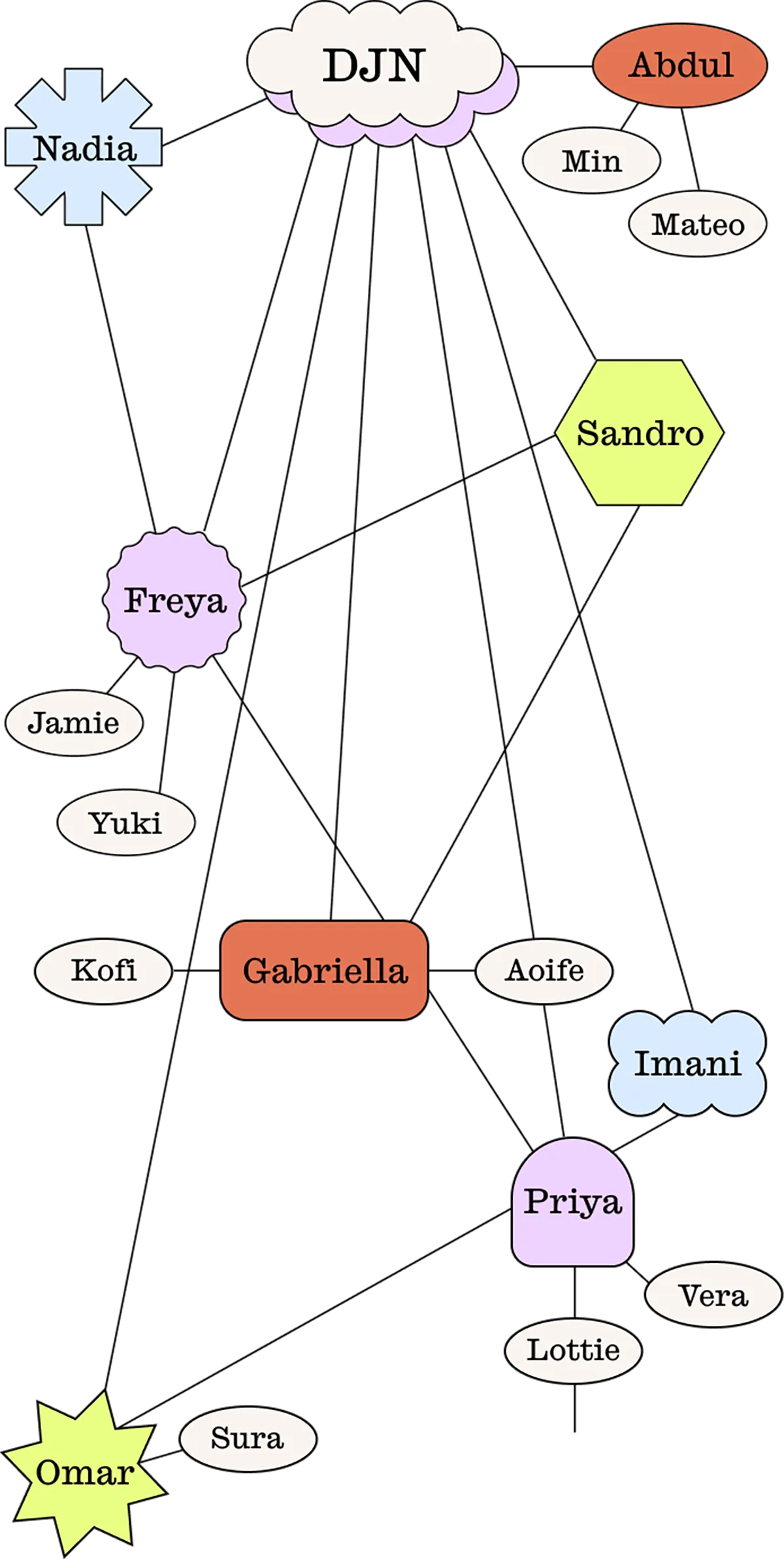
Our mission is to guide our audience towards meaningful action at the end of each issue, working with our Advisory Board to spotlight a group or organisation doing important work for the community we are all a part of.
We invite you to read this section and hear from the Disability Justice Network (DJN). Please take the time to read, learn and rally behind them with us.
Our mission is to guide our audience towards meaningful action at the end of each issue, working with our Advisory Board to spotlight a group or organisation doing important work for the community we are all a part of.
We invite you to read this section and hear from the Disability Justice Network (DJN). Please take the time to read, learn and rally behind them with us.
Support the Disability Justice Network
Our mission is to guide our audience towards meaningful action at the end of each issue, working with our Advisory Board to spotlight a group or organisation doing important work for the community we are all a part of.
We invite you to read this section and hear from the Disability Justice Network (DJN). Please take the time to read, learn and rally behind them with us.
Our mission is to guide our audience towards meaningful action at the end of each issue, working with our Advisory Board to spotlight a group or organisation doing important work for the community we are all a part of.
We invite you to read this section and hear from the Disability Justice Network (DJN). Please take the time to read, learn and rally behind them with us.
Enter
Article
read
more
Enter
Article
read
more
Enter
Article
Meet the contributors
We couldn’t have put this first issue together without the leap of faith our team, advisory board and contributors took with us – thank you.
Additionally, a huge thank you to Lauren Frost, Lucie Greene, Domenic Iaria, Erin Lyon, Connor O'Brien, Rena Ou Yang and Ella Shi for giving us their expertise and advice.
Contributors
Meet the contributors
We couldn’t have put this first issue together without the leap of faith our team, advisory board and contributors took with us – thank you. Additionally, a huge thank you to Lauren Frost, Lucie Greene, Domenic Iaria, Erin Lyon, Connor O'Brien, Rena Ou Yang and Ella Shi for giving us their expertise and advice.
Alex Creece
Writer
@roguedyke
Amity Mara
Podcast Interviewee
-
Artie Carden
Content Creator
@artiecarden
Ashley Apap
Video Creator
@ashleycrapap
Dominique Acciarito
Video Interviewee
@thespooniesocietyAU
Em Jensen
Photographer
@emjensencreative
Emilia Schnall
Photo Essay Interviewee
@missemiliamusic
Fi Macrae
Content Creator
@privatepartscommunity
Grace Taylor
Illustrator
@gracetaylorillustration
Helene Hill
Video Interviewee
@thespooniesocietyAU
Iman Rahman
Content Creator & Video Interviewee
@alilbitofaith
Julia Bak
Writer
@mugworts
Kaitlyn Blythe
Video Interviewee
@blythebyname
Kate Marshall
Podcast Interviewee
@hacsu
Katie Zhou
Illustrator
@katiezhoudesign
Kenzie TTH
Content Creator
@sicksadgirlz
Khadija Gbla
Video Interviewee
@khadija_gbla
Leon Harper
Podcast Interviewee
@youngworkersvic
Lou Wall
Video Creator
@thelouwall
Michael Sun
Playlist Creator
@michael.pdf
Nory Gretz
Photo Essay Interviewee
@norygretz
Renay Barker-Mulholland
Writer
@firstnations_feminist
Róisín McGee
Podcast Interviewee
@roisin.mcgee
Rosa Mercuriadis
Content Creator
@sicksadgirlz
Sophie Aylmore
Video Interviewee
@sophie_aylmore
Thomas Feng
Photographer
@thomasfengg
Tori Hobbs
Video Interviewee & Playlist Creator
@jackiebyjoanne
Alex Creece
Writer
@roguedyke
Amity Mara
Podcast Interviewee
-
-
Artie Carden
Content Creator
@artiecarden
Ashley Apap
Video Creator
@ashleycrapap
-
Dominique Acciarito
Video Interviewee
@thespooniesocietyau
Em Jensen
Photographer
@emjensencreative
Emilia Schnall
Photo Essay Interviewee
@missemiliamusic
Fi Macrae
Content Creator
@privatepartscommunity
Grace Taylor
Illustrator
@gracetaylorillustration
-
Helene Hill
Video Interviewee
@thespooniesocietyau
Iman Rahman
Content Creator& Video Interviewee
@alilbitofaith
Julia Bak
Writer
@mugworts
Kaitlyn Blythe
Video Interviewee
@blythebyname
-
Kate Marshall
Podcast Interviewee
@katemarshall82
Katie Zhou
Illustrator
@katiezhoudesign
Kenzie TTH
Content Creator
@sicksadgirlz
Khadija Gbla
Video Interviewee
@khadija_gbla
Leon Harper
Podcast Interviewee
@leon.ash.harper
-
Lou Wall
Video Creator
@thelouwall
Michael Sun
Playlist Creator
@michael.pdf
-
Nory Gretz
Photo Essay Interviewee
@norygretz
Renay Barker-Mulholland
Writer
@firstnations_feminist
Róisín McGee
Podcast Interviewee
@roisin.mcgee
Rosa Mercuriadis
Content Creator
@sicksadgirlz
Sophie Aylmore
Video Interviewee
@sophie_aylmore
Thomas Feng
Photographer
@thomasfengg
Tori Hobbs
Video Interviewee & Playlist Creator
@jackiebyjoanne
Keep in touch
Thank you for reading this issue of Rally Magazine.